my journey in the realm of general medicine department
The General Medicine Department serves as the cornerstone of healthcare, dealing with a diverse range of medical conditions.
Embarking on my journey within the realm of the General Medicine Department has been both enlightening and transformative. This department, often considered the backbone of healthcare, encapsulates the essence of medical practice by addressing a myriad of medical conditions and providing a holistic approach to patient care.
From the outset, I was immersed in the art of history-taking, recognizing its pivotal role in unraveling the intricate tapestry of a patient's health. Learning to navigate through the nuances of each patient's narrative, I discovered that the subtleties often held the key to understanding the onset and progression of their ailments.
The clinical examinations became a canvas where I could observe and interpret the manifestations of various medical conditions. Each palpation, auscultation, and observation became a piece of the diagnostic puzzle, contributing to the broader understanding of the patient's health status.
Case 1
During my op day case presented at the outpatient department
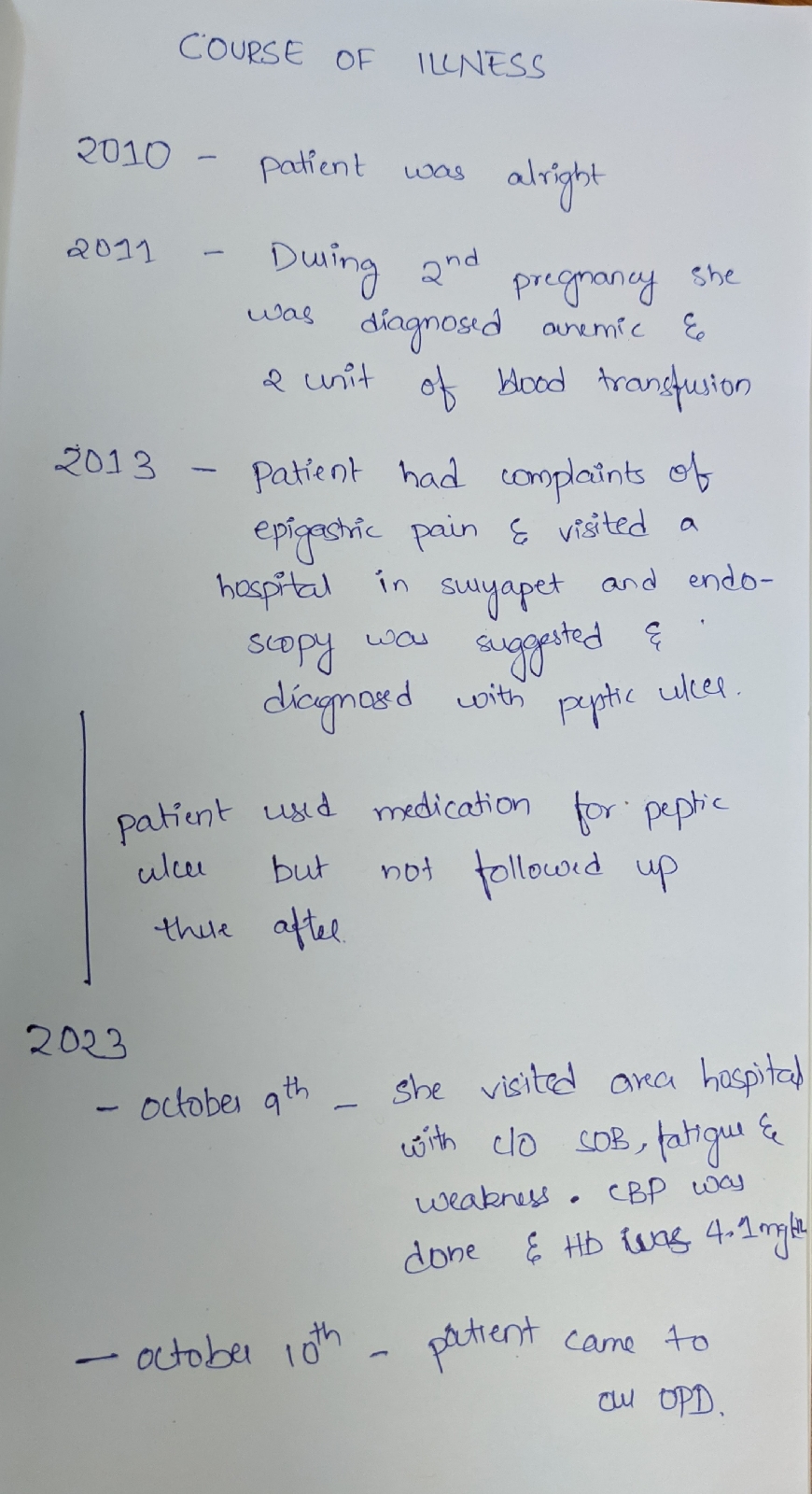
The 30-year-old female patient's complaints of fatigue, weakness, and shortness of breath over the past 12 years serve as a compelling example of the challenges faced by both patients and healthcare professionals
One of the fundamental learning points from this case is the significance of a comprehensive history taking process. The patient's journey from being asymptomatic for 12 years to developing symptoms requires a meticulous exploration of her medical history, lifestyle, and systemic review. The gradual onset of symptoms, such as cold intolerance, constipation, weight fluctuation, burning micturition, and malena, Indicates a potential underlying systemic issue
The clinical examination plays a pivotal role in identifying visible manifestations of the patient's condition. In this case, the presence of paller raises concerns about a possible anemic state. necessitating further investigation. General examination, including the absence of ictarus, cyanosis, and edema, provides crucial information for differential diagnosis.
Vital signs are essential indicators of the patient's overall well-being. Within normal ranges in this case, they provide initial reassurance, but the persistence of symptoms demands a deeper exploration.
Systemic examinations, such as cardiovascular, respiratory neurological, and abdominal assessments, are invaluable tools in the diagnostic process. While cardiovascular and respiratory systems appear unremarkable, abdominal softness and non-tenderness raise questions about the origin of the patient's symptoms.
The provisional diagnosis of anemia under evaluation guides the next steps in patient management. The chosen Investigations, including a complete blood count, iron studies, thyroid function tests, stool examination, and urinalysis, align with the presented symptoms. This approach reflects the department's commitment to a systematic and evidence-based diagnosis, ensuring a thorough exploration of potential causes
This case highlights the Interdisciplinary nature of patient care within the General Medicine Department
Blog link
https://bharathkumarrollno108.blogspot.com/2023/10/30-f-with-complaints-of-sob-on-and-off.html
Pajr link
https://chat.whatsapp.com/Gsd7pWIkHu6EmkQLdVFJVf
[13/10, 10:42 am] bharath kumar: Sir initially patient hb was 4.1 mg/dl after 1 unit of PRBC transfusion now her hb is 6.5 mg/dl
Patient is doing well with no complaints sir
[13/10, 2:33 pm] Dr.Rakesh Biswas GM HOD: What's the cause for her anemia?
[13/10, 4:08 pm] bharath kumar: Blood loss(Menorrhagia) sir and
She is diagnosed with peptic ulcer 12 years back sir and used medication on and off
[13/10, 4:14 pm] Dr.Rakesh Biswas GM HOD: How much of blood loss? When documented?
Case 2
a 60- year-old female patient presented with a perplexing puzzle-generalized body pains persisting for the past 2 years. This case illuminates the intricate nature of chronic pain and the challenges faced by healthcare professionals in deciphering its underlying causes.
History of Present Illness (HOPI):
The patient, initially asymptomatic 2 years ago, gradually developed generalized body pains accompanied by multiple joint pains and lower backache. Complaints of joint stiffness and difficulty rising from a sitting position added layers to the clinical picture. Remarkably, no history of trauma, fever, or tenderness was reported.
Past Medical History:
The patient's medical history reveals a complex interplay of conditions, including hypertension, diabetes, epilepsy, cerebrovascular accident (CVA), coronary artery disease (CAD), and thyroid disorders. A history of blood transfusion a decade ago and prior surgeries, including hysterectomy and percutaneous nephrolithotomy (PCNL) for renal calculi, further complicates the narrative.
Personal History:
The patient maintains a mixed diet with normal appetite and adequate sleep. However, the occasional indulgence in smoking chutta adds an additional layer to the health profile.
Clinical Examination:
The general examination unveils a patient who is conscious, coherent, and well-oriented to time, place, and person. She is moderately built and nourished, with no apparent signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy, or generalized edema.
Vital Signs:
Vital signs, including temperature, pulse rate, blood pressure, and oxygen saturation, fall within normal ranges, providing initial reassurance but prompting a deeper investigation into the root cause of the chronic pain.
Systemic Examination:
Cardiovascular and respiratory systems appear normal with no murmurs or respiratory abnormalities. Neurological findings reveal no focal deficits, while the abdominal examination demonstrates softness and non- tenderness.
This intricate case poses a diagnostic challenge, requiring a systematic approach to unravel the underlying factors contributing to the patient's chronic pain. Further investigations, such as imaging studies, blood tests, and consultations with specialists in rheumatology or orthopedics, may be warranted.
In conclusion, this case exemplifies the complexity inherent in general medicine, where the convergence of various medical conditions and lifestyle factors requires a meticulous and comprehensive evaluation. It underscores the need for healthcare professionals to navigate through a myriad of symptoms, histories, and examinations to provide patient- centered care and formulate an effective management plan
Blog link
https://bharathkumarrollno108.blogspot.com/2023/10/a-60yr-old-female-came-with-complaints.html
Pajr link
https://chat.whatsapp.com/L2Q422762Q88ctKriIRSmI
[10/10, 9:16 pm] Dr.Rakesh Biswas GM HOD: Does she have polyarthritis?
Share each joint examination findings
[10/10, 11:35 pm] bharath kumar: Ok sir
[11/10, 10:38 am] bharath kumar: Proximal interphalangeal joints of left and right hands
-No swelling
-no tenderness
-limitation of movements present
Metacarpophalangeal joints of left and right hand
-No swelling
-no tenderness
-No limitation of movements
Wrists,elbows, shoulders and knees of both sides
-No swelling
-No tenderness
-No limitation of movements
[11/10, 2:44 pm] Dr.Rakesh Biswas GM HOD: No arthritis at all?
[11/10, 5:46 pm] bharath kumar: There is stiffness and limitation of movements of interphalangeal joints sir
Some other cases i have seen and lucky enough to help my colleagues
Blog links
https://bharathkumarrollno108.blogspot.com/2023/10/a-40yr-female-came-with-complaints-of.html
https://bharathkumarrollno108.blogspot.com/2023/10/a-65-year-old-came-to-casuality-with-co.html
An interesting literature was contributed in this patient
[09/10, 9:39 am] Dr.Rakesh Biswas GM HOD: Why did this diabetic land up in Ckd and dialysis within 7 years while there are many diabetics in our campus with 20 years and no complications or organ involvement? Can you try to look for the factors that make this patient different from them?
[09/10, 9:49 am] bharath kumar: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6014002/#:~:text=During%2024%2Dmonth%20follow%2Dup,and%20higher%20systolic%20blood%20pressure.
[09/10, 9:50 am] bharath kumar: In sum, within a large, contemporary population of adults with mild-to-moderate CKD, accelerated progression of kidney dysfunction within 2 years affected ~ 1 in 4 patients with diabetes and ~ 1 in 7 without diabetes. Regardless of diabetes status, the independent predictors of fast CKD progression included proteinuria, elevated systolic blood pressure, heart failure, anemia, and age ≥ 80 years. Age 18–49 years was also a predictor in those with diabetes, while additional predictors in patients without diabetes included smoking history, prior ischemic stroke, prior pacemaker implantation, and HDL cholesterol < 60 mg/dL. These findings may help in identifying the subset of patients who may benefit from more frequent monitoring of eGFR to identify fast CKD progression or proteinuria and subsequent intervention to potentially retard further loss of kidney function and other potentially associated adverse clinical outcomes such as cardiovascular events.
[09/10, 9:52 am] Dr.Rakesh Biswas GM HOD: Which one of these match this patient?
[09/10, 9:52 am] bharath kumar: Will check and report back to you sir
[09/10, 10:03 am] bharath kumar: As mentioned age 18-49 years, it is also a predictor of accelerated progression sir
https://bharathkumarrollno108.blogspot.com/2023/10/35-year-old-female-patient-with-fever.html
Procedures performed
Assisted in central line
In conclusion, I want to convey my heartfelt thanks for the opportunities and experiences I have gained in the General Medicine Department. This chapter has been a stepping stone in my career, and I am eager to carry forward the lessons learned as I continue to grow both personally and professionally.



Comments
Post a Comment