This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input
30 year old female patient came to opd with complaints of fatigue , weakness and SOB since 12 years
HOPI
patient is apparently asymptomatic 12 years then she developed SOB (grade 2-3)on and off associated with
fatigue and weakness
C/o cold intolerance
C/o constipation (once in 2-3 days)
C/o weight fluctuation since 1 year
C/o burning micturition
C/o malena since 3 months
C/o bloating
No H/o fever,nausea, vomiting,cold, cough
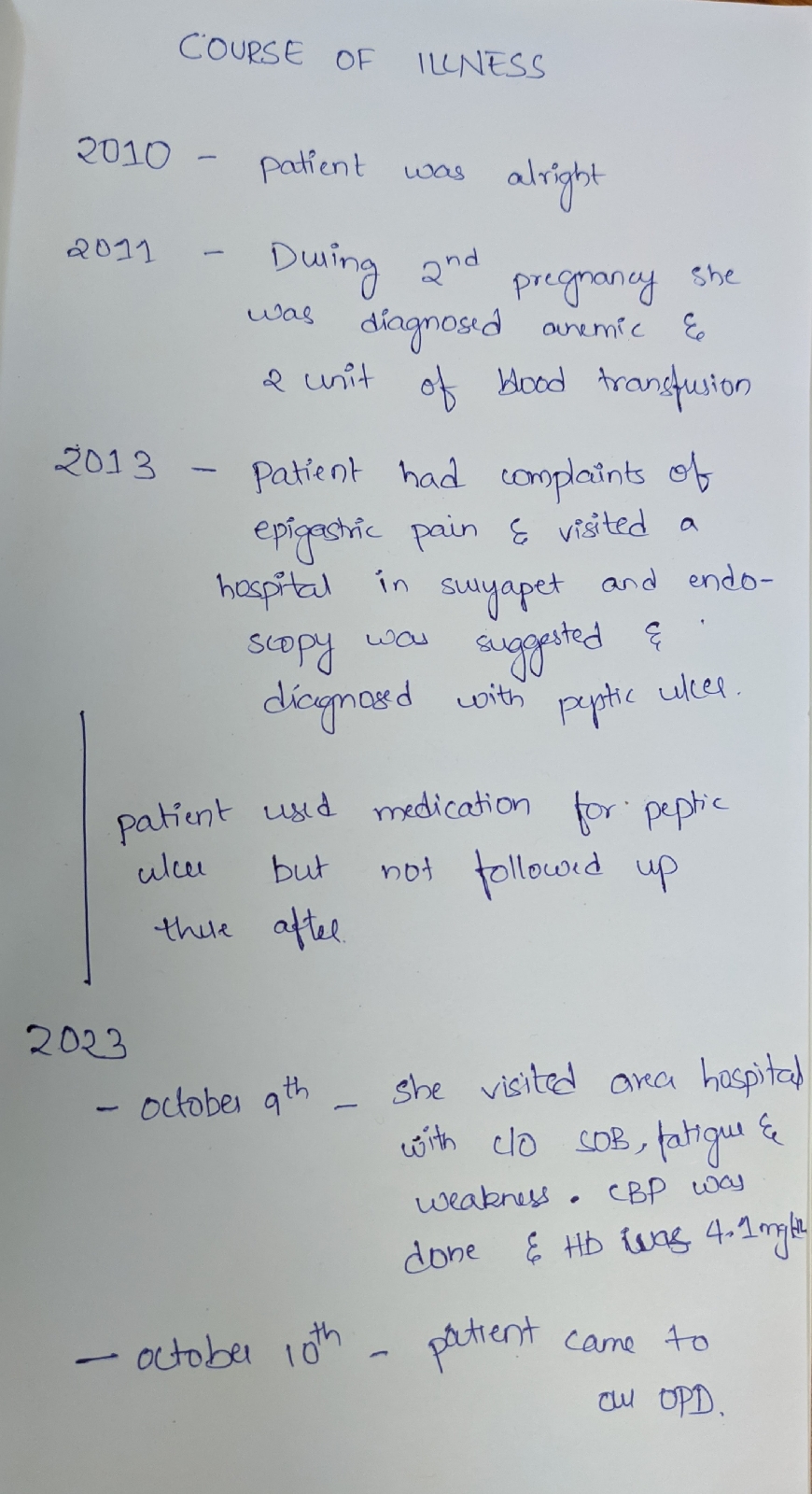
COURSE OF ILLNESS
Past history
N/k/c/o HTN,DM,CAD,asthma,TB, epilepsy,CVA
H/o 2 units of blood transfusion done 12 years ago during 2nd pregnancy antenatally, Allergic reaction noted during 1st unit of transfusion and medication given
Tubectomy done 10 years back
Personal history:
Diet mixed
Appetite decreased
Sleep inaequate
Bowel and bladder irregular
No addictions
No significant family history
Menstrual history
Age of menarche - 13 years
Menstrual cycle - 7-8/30
Uses 1 pad per day
General examination
Patient is c/c/c well oriented to time place person
Moderately built and nourished
Pallor present
No signs of icterus cyanosis clubbing lymphadenopathy generalized edema
Vitals :
Temperature 97.5
PR 83 bpm
BP 130/80 mmhg
RR 21cpm
Spo2 98 at ra
Systemic examination
CVS - S1 S2 Heard no murmurs
RS - BAE + NVBS
CNS : NFND
P/A : soft,non tender
Provisional diagnosis
Anemia under evaluation
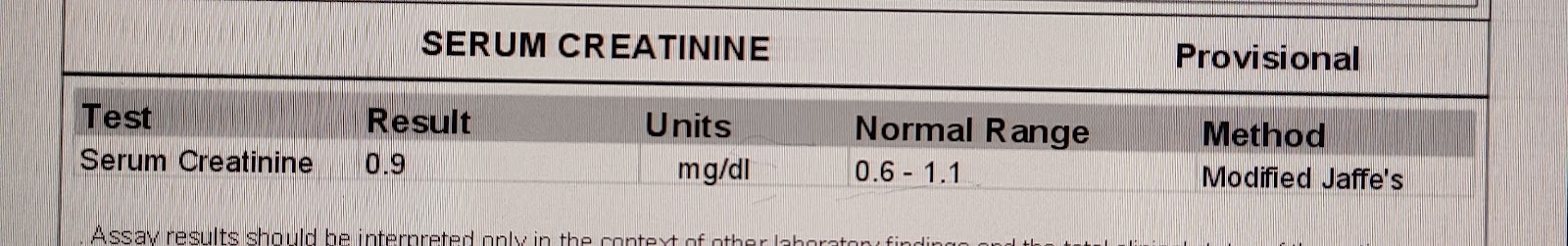
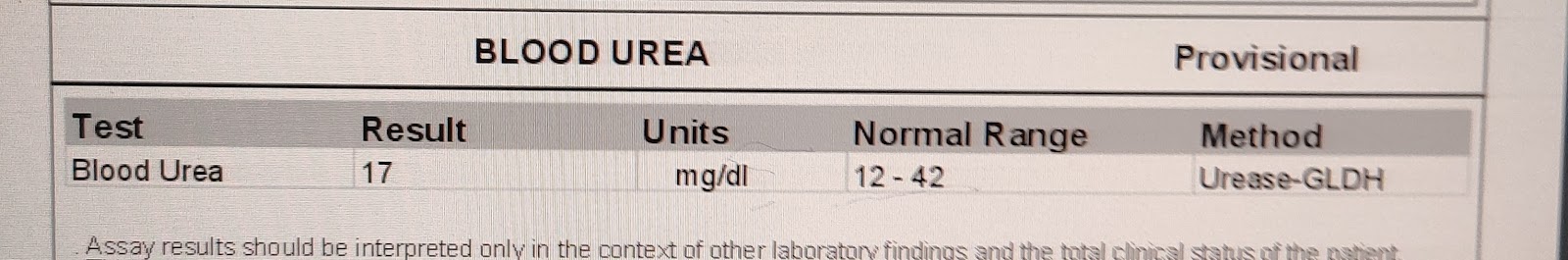
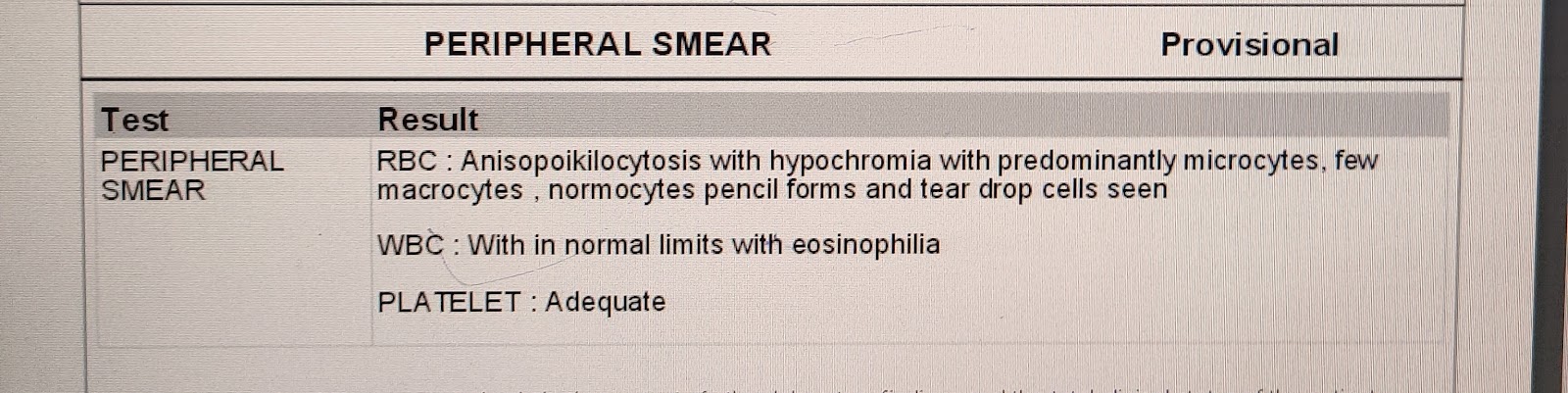
Investigations
USG
impression
E/o 60x45mm fibroid noted in the posterior myometrium of the uterus
Grade 1 fatty liver
FINAL DIAGNOSIS
Iron deficiency Anemia 2° to blood loss with dilated cardiomyopathy with intramural fibroid
TREATMENT
TAB OROFER XT PO/OD
1 UNIT OF PRBC TRANSFUSION DONE
OSCE:
Question 1
What additional questions would you ask to explore the patient's complaint of burning micturition?
Answer
To explore the complaint of burning micturition, I would ask additional questions such as the frequency of urination, any associated pain, presence of blood in the urine, history of urinary tract infections, and any recent changes in urinary habits. Additionally, inquiring about any history of gynecological issues or recent sexual activity could be relevant.
Question 2
How would you investigate and manage a patient with iron deficiency anemia secondary to blood loss and dilated cardiomyopathy?
Answer
To investigate and manage a patient with iron deficiency anemia secondary to blood loss and dilated cardiomyopathy, I would initiate a comprehensive approach. This includes further evaluation of the source of blood loss through endoscopic studies (such as colonoscopy), addressing the anemia with iron supplementation, and collaborating with cardiology for the management of dilated cardiomyopathy. Regular follow-ups and adjustments to the treatment plan based on the patient's response would be crucial.
Question 3
Given the patient's vitals, what further assessments or investigations would you consider to evaluate the severity of the anemia and its impact on the cardiovascular system?
Answer
Given the patient's vitals, I would consider further assessments such as a complete blood count (CBC) to evaluate the severity of anemia, an electrocardiogram (ECG) and echocardiogram to assess cardiac function, and possibly cardiac biomarkers to gauge cardiac stress. Continuous monitoring of vital signs and serial assessments would be important to track the patient's response to treatment.
Question 4
What are the potential complications of untreated iron deficiency anemia, and how might these be exacerbated in a patient with a concurrent peptic ulcer?
Answer
Untreated iron deficiency anemia can lead to complications such as cardiac strain, impaired cognitive function, and compromised immune function. In a patient with a concurrent peptic ulcer, these complications may be exacerbated due to the ongoing blood loss from the ulcer. The combination of gastrointestinal bleeding and iron deficiency places additional stress on the cardiovascular system and can further compromise the patient's overall health. Timely diagnosis and management of both conditions are essential to prevent complications.
Question 5
Explain the relationship between iron deficiency anemia and peptic ulcers. How might peptic ulcers contribute to the development of iron deficiency anemia?
Answer
Peptic ulcers can contribute to iron deficiency anemia through chronic blood loss. The ulceration of the gastrointestinal mucosa, commonly in the stomach or duodenum, can result in slow, chronic bleeding. This occult blood loss may not be immediately evident but can lead to a gradual depletion of iron stores, eventually causing iron deficiency anemia. Monitoring for signs of gastrointestinal bleeding and performing diagnostic tests such as endoscopy can help identify and manage peptic ulcers as part of the comprehensive approach to treating iron deficiency anemia.