This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input
30 year old female patient came to opd with complaints of fatigue , weakness and SOB since 12 years
HOPI
patient is apparently asymptomatic 12 years then she developed SOB (grade 2-3)on and off associated with
fatigue and weakness
C/o cold intolerance
C/o constipation (once in 2-3 days)
C/o weight fluctuation since 1 year
C/o burning micturition
C/o malena since 3 months
C/o bloating
No H/o fever,nausea, vomiting,cold, cough
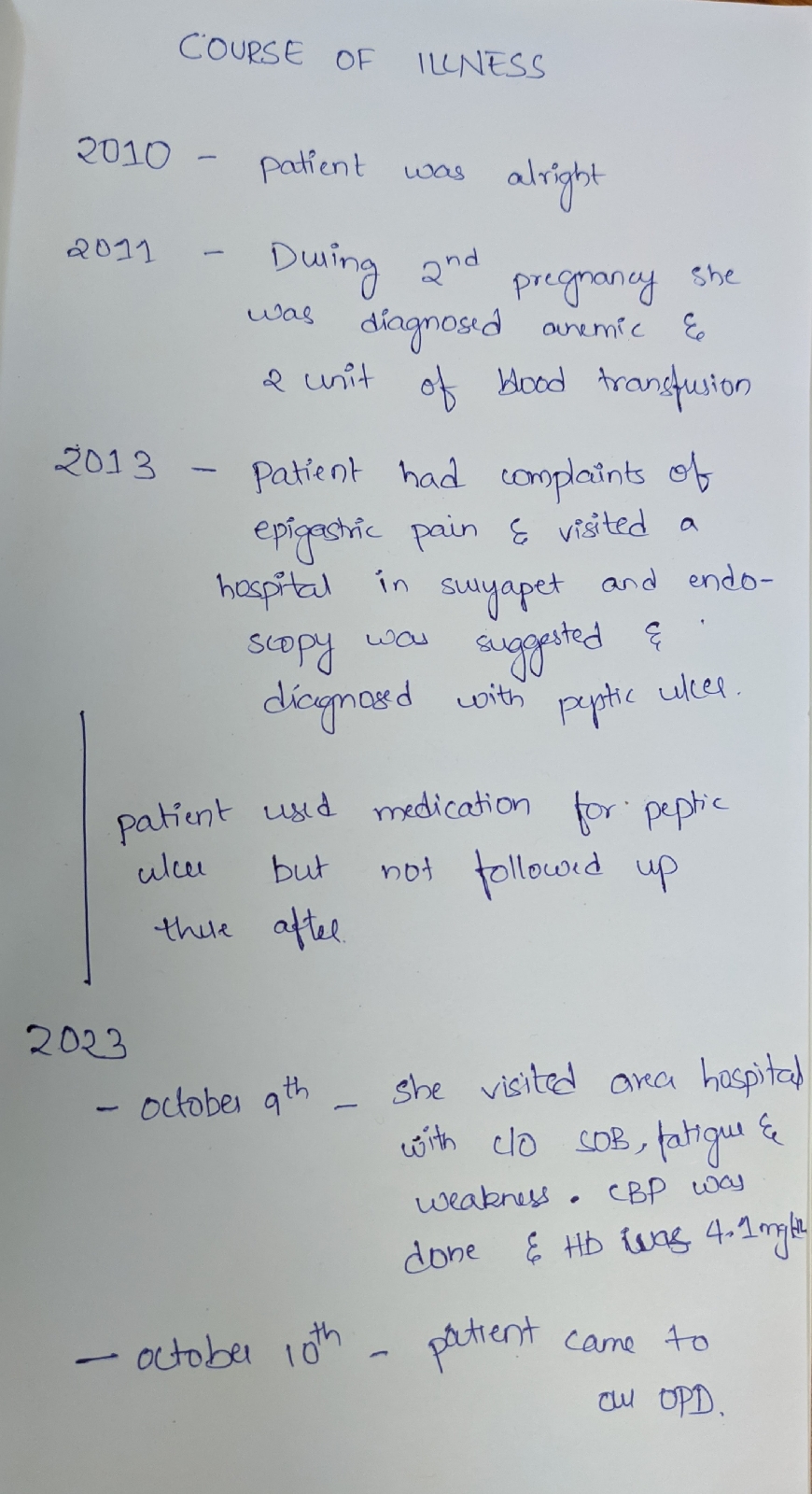
COURSE OF ILLNESS
Past history
N/k/c/o HTN,DM,CAD,asthma,TB, epilepsy,CVA
H/o 2 units of blood transfusion done 12 years ago during 2nd pregnancy antenatally, Allergic reaction noted during 1st unit of transfusion and medication given
Tubectomy done 10 years back
Personal history:
Diet mixed
Appetite decreased
Sleep inaequate
Bowel and bladder irregular
No addictions
No significant family history
Menstrual history
Age of menarche - 13 years
Menstrual cycle - 7-8/30
Uses 1 pad per day
General examination
Patient is c/c/c well oriented to time place person
Moderately built and nourished
Pallor present
No signs of icterus cyanosis clubbing lymphadenopathy generalized edema
Vitals :
Temperature 97.5
PR 83 bpm
BP 130/80 mmhg
RR 21cpm
Spo2 98 at ra
Systemic examination
CVS - S1 S2 Heard no murmurs
RS - BAE + NVBS
CNS : NFND
P/A : soft,non tender
Provisional diagnosis
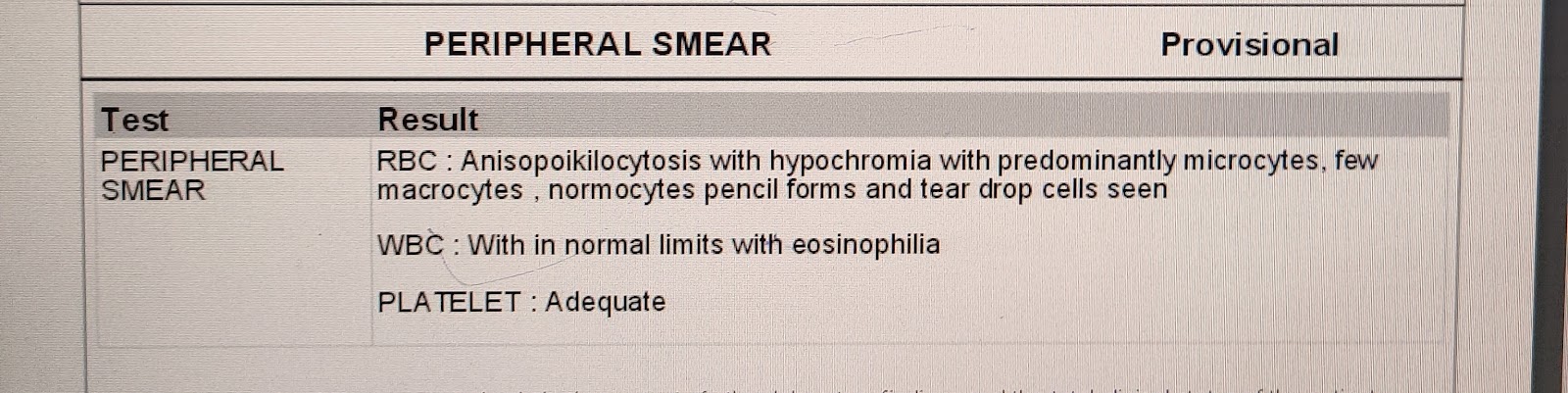
Anemia under evaluation
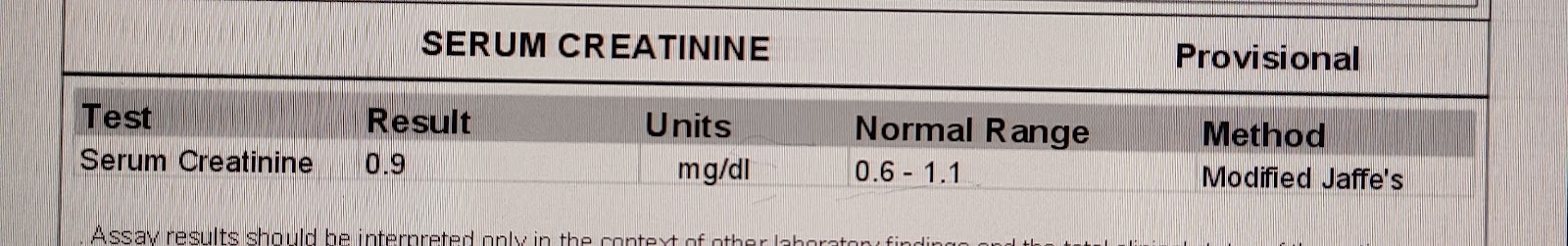
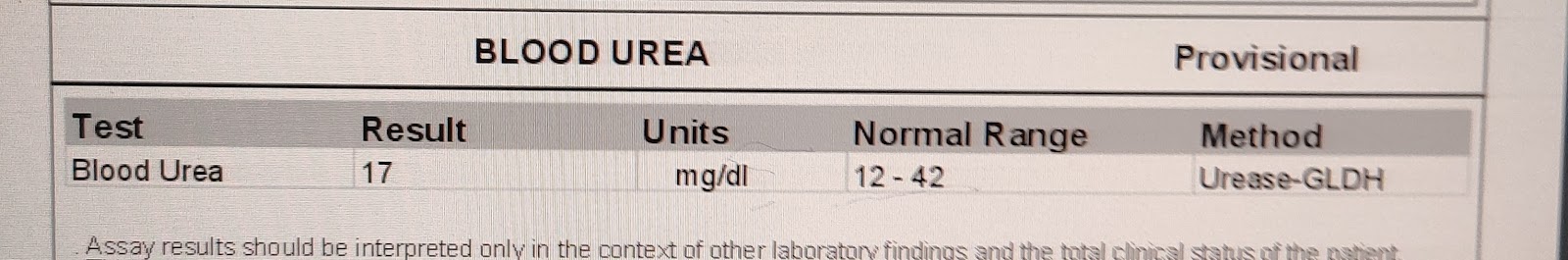
Investigations
USG
impression
E/o 60x45mm fibroid noted in the posterior myometrium of the uterus
Grade 1 fatty liver
FINAL DIAGNOSIS
Iron deficiency Anemia 2° to blood loss with dilated cardiomyopathy with intramural fibroid
TREATMENT
TAB OROFER XT PO/OD
1 UNIT OF PRBC TRANSFUSION DONE



















Comments
Post a Comment