This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 80 year old male patient was brought to casualty(i.e4/10/2022)
CC:
Shortness of breath since 4days
Fever since 4days
Cough since 3days
Loose stools 2days
History of present illness:
Patient was apparently symptomatic 1 month back then he developed anuria for which he was admitted in a hospital for a day foleys was placed and medication was given for 10 days ,then patient developed shortness of breath four days back which was insidious in onset gradually progressed from grade 2 to grade 4 (mmrc),no postural variation ,no history of suggestive of paroxysmal nocturnal dyspnoea, chest pain ,associated with cold and cough ,cough was productive, sputum mucoid,whitish,copious and not blood tinged and has a history of fever which was intermittent ,on and off ,no diurnal variation and associated with loose stools and burning micturition ,loose stools since two days 3 to 4 episodes per day ,non-bulky not associated with pain abdomen ,non-bloodstained .
This developed after drinking beer(2bottles)
No similar complaints in the past
Not a know case of DM,ASTHMA,HTN,EPILEPSY,TB
H/O pasaramandu done 30 years back
Personal history:
Diet:mixed
Appetite:normal
Bowel and bladder movements:irregular (loose stools), decreased urine output since 1month
Addictions: alcohol consumption from past 30years (daily quarter) stopped 1 month back , last intake was 5 days back
Smoking (Chutta) daily 4-5 , stopped 5 years back
No know allergies
Family history:
No relevant family history
General Examination:
Patient was not C/C/C not oriented to time,place and person
Pallor -absent
Icterus-absent
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Edema-absent
Vitals:
PR:87bpm
BP:140/70mm Hg
RR:35cpm
Spo2:94%
RBS: 228 mg/dl
Systemic examination:
RS:
Inspection :
R. L
Supraclavicular area :hollow. Normal
Infraclavicular area. :Crowding Normal
Position of trachea :prominent SCM on rigth side
Position of Apex beat :5 th ics
Chest : asymmetry
Increased AP diameter on left side
Palpation:
Confirmed inspiratory finding
Trachea deviated to rigth
Irregular chest movements
Percussion:
Auscultation :
Decreased air entry on rigth side
Normal vesicular breath sounds
CVS:
Apex beat at 5th ics at midclavicular line
S1,S2 heard
Per abdomen:
Scaphoid
Scar + rt side( h/o? hernia sx)
No Tenderness
No organomegaly
CNS:
Involuntary movements (? Fasiculations + at rt and lt proximal lowerlimb)
Tone : normal in all limbs
Reflexes:
Rt. Lt.
B. +++ ++
T. ++ +
K. ++ ++
A. ++ ++
P. Mute
Intially pulmonology consultation done :
Suggested Bipap with peep 5 and fiO2 0.3
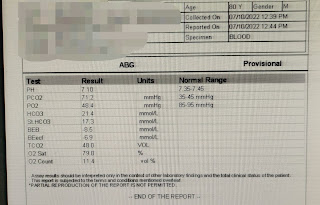
Investigations:
4/10/22:
6/10/22:
7/10/22:
8/10/22:


Provisional diagnosis:
Altered sensorium (hypoactive) secondary to type 2 respiratory failure,?uremic encephalopathy Non oliguric aki with rt upper lobe fibrosis(?TB)
Treatment:(4/10/22)
1. IV fluids -NS,RL
2.nebulization with milk and salbutamol
3. 25D with 10units HAI inj stat
4. Watch for hypoglycemia
5.inj lasix 40mg iv stat
6. 25D infusion /10ml/hr until 150ml /dl
7. Hourly GRBS monitoring
8. Monitor vitals hrly charting
9.strict i/o charting
10.syp. grillinctus 15ml/oral/BD
5/10/22:
Our patient was fighting with ventilator which has objective evidence of RR 56CPM. So we paralysed him and controlled his RR @ 24cpm.
O/E:
Pt was on mechanical ventilation
PR:78bpm
BP:110/80mmhg
CVS: S1,S2 heard
RS: decreased breath sounds in inframammary area rigth side
Left side NVBS
Crepts rt.axillary
P/a: soft nontender,scaphoid , non distended
CNS: no focal neurological deficits
Treatment:(5/10/22)
1.Iv fluids -75ml/hr ,ns rl
2.inj. monocef -1gm/iv/BD -8am 8pm
3.inj. midazolam -4ampules @5ml/hr
4.inj . Atracurium-2 ampules+45ml NS
5. 25D infusion @15ml/hr Inc or dec to GRBS
6.Air bed
7. Frequent position changing
8.ryles tube milk 100ml, water 100ml
9. Nebulization budecort BD 12 hrly,asthalin
10.inj. pan 40mg iv OD
11.inj lasix 40mg iv BD
12.Tab. dolo 650mg sos(>100F)
6/10/22:
O/E:
Pt on mechanical ventilation
GCS-E1VTM1
Afebrile
PR:89bpm
Irregular rhythm
BP:120/80mmhg
GRBS:220mg/dl
CVS: S1 S2 heard
RS: decreased breath sounds in inframammary area rigth side
Left side NVBS
Crepts rt.axillary
P/a: soft nontender,scaphoid , non distended
CNS:
R. L
B. +. +
T. +. +
K. -. +
A. +. +
P. Mute Mute
Treatment:(6/10/22)
1.iv fuilds @125ml/hr rl,ns
2.inj. monocef 1g/iv/bd
3.25D infusion @5ml/hr
4.inj. pan 40mg iv OD
5.inj. lasix 40mg iv bd
6.ryles tube milk 100ml, water 100ml
7.air bed
8. Frequent position changing 2hrly
9.neb budecort BD 12 hrly, asthalin 3hrly
10.tab dolo 650mg sos
11. Vitals monitor hrly
12.GRBS charting
13.strict i/o charting
14. Inform SOS
Plan for hemodialysis (rt femoral line )

Central line (rt femoral vein)
7/10/22:
8/10/22:
O: Patient on Mechanical Ventilator
Mode: CPAP VC
RR total: 40
FiO2 : 30
PEEP: 7
Temp-99.5°F
BP-120/70 MMHG
PR-80 BPM
RR-24 CPM
CVS-S1S2+
RS: BAE+
Crepts + Left infra axillary added sounds @ left infclavicular, right mammary
P?/A : soft, non- tender
SPO2 - 98%
GRBS: 138mg/dl
GCS: E1VtM4
A:
Altered Sensorium ( hypoactive) secondary to T-II respiratory failure?
Uremic Encephalopathy
Non Oliguric AKI? AIN? ATN with Right Upper Lobe Fibrosis
Post Hemodialysis (1 session on 06/10/22 )
P:
1. IVF NS and RL @ 50mL /hr
2. INJ. MONOCEF 1g/ IV/BD
3. INJ. LASIX 80mg /IV /BD
4. Ryles feed - milk (100 mL+ protein powder) 4th hourly
water - 100mL 6th hourly
5. TAB. AZITHROMYCIN 500mg /RT/OD
6. TAB. DOLO 650mg/RT/SOS if temp. more than 101F
7. Air bed
8. Nebulisation
- Budecort /BD/12th hourly
- Asthalin / TID/ 8th hourly
9. Frequent position change 2nd hourly
10. Monitor vitals BP, Temp, PR, RR, SpO2 hourly
11. GRBS charting 2nd hourly
12. Strict I/O charting
13. Inform SOS
















































Comments
Post a Comment